This 90-minute presentation will begin by discussing the physiology of the human upper airway and how it responds to positive intraluminal pressure. The impact of positive airway pressure on the patency and flow of the pharyngeal airway will be discussed, as will the effect of lower expiratory positive airway pressure (EPAP).
The second talk will address the published results of multiple attempts to lower EPAP to make PAP more comfortable. These include BiPAP, C-Flex, and expiratory pressure relief (EPR), all of which failed to improve adherence to PAP.
Finally, the third presentation will address the concept of lowering pressure during all of inspiration and most of expiration, with full pressure being delivered only towards the end of expiration. The effect of this pressure algorithm on efficacy in treating OSA and patient comfort will then be discussed.
A Q&A session will follow the presentation.
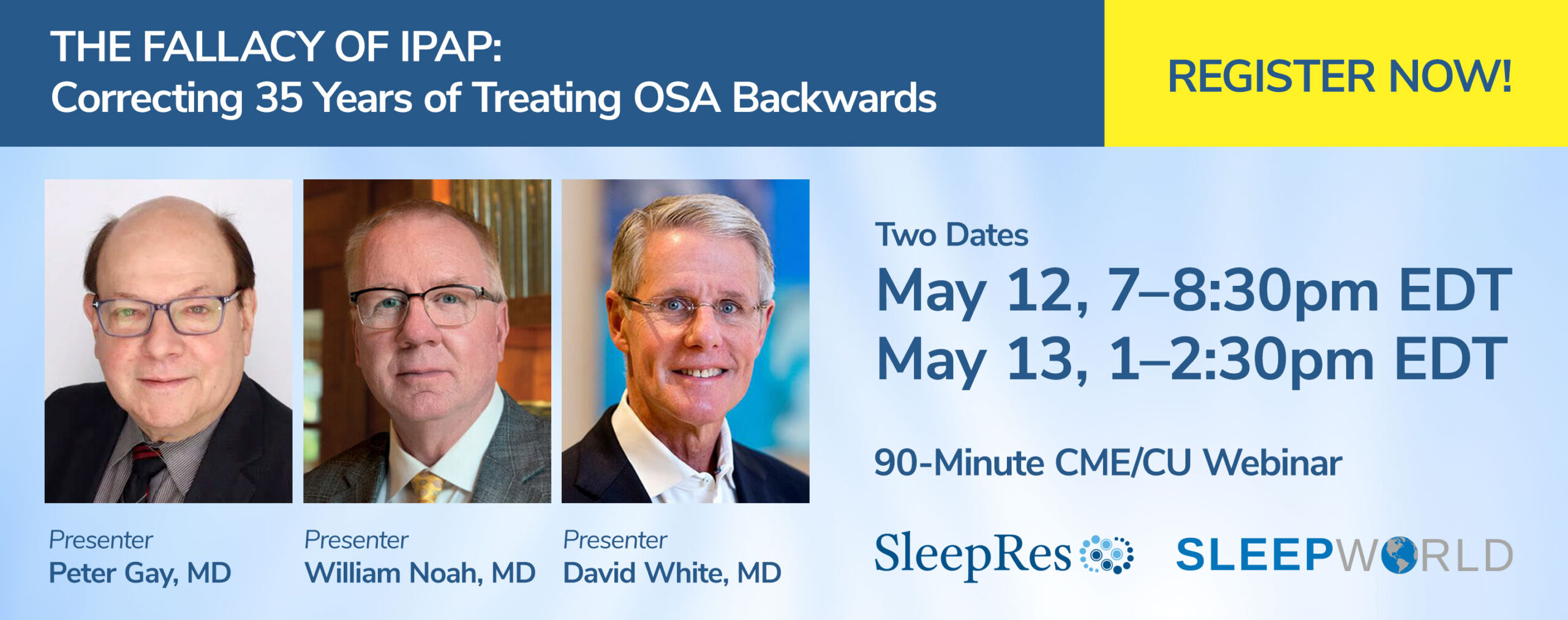
Webinar Series
This is the eighth and final webinar in the Discoveries in Sleep Apnea Series.
- Complex Sleep Apnea –
20 Years On! - KairosPAP(KPAP) Pressure at the Right Time –
The Future of PAP Therapy for OSA - Sleep Apnea and Cardiovascular Disease:
Could Excessive CPAP Explain the Negative Clinical Trials? - APAP: Challenges and Opportunities
- Central Apnea: Back to Basics
- Obesity Hypoventilation Syndrome for the Clinician
Earn 1.50 CME, ADA, CSTE, CRCE
Learning Objectives
1. To educate the audience regarding the human pharyngeal airway and how it responds to positive pressure and reductions in positive pressure, particularly during expiration and sleep.
2. To review the published literature on the effects of lowering expiratory pressure on satisfaction and adherence to CPAP.
3. To propose a new algorithm for pressure delivery with lower inspiratory and expiratory pressure (other than at end expiration) and the comfort and efficacy of such an algorithm in treating OSA.
Accreditation
Application will be made for 1.5 credit hours for CME, Dental, CSTE, and CRCE.
There is no charge for this webinar.
About the Speakers
David P. White, MD, was the first Gerald E. McGinnis Professor of Medicine at Harvard Medical School, where he trained many of today’s leaders in sleep medicine. He is a former editor-in-chief of the journal SLEEP, president of the American Academy of Sleep Medicine, and chairman of the NIH’s sleep research task force, He also served as Chief Medical Officer for Respironics and Philips Respironics until 2013. With 300 publications, he continues his primary research at Harvard focusing on the pathophysiology of sleep breathing disorders.
Peter Gay, MD, received his B.A. from Middlebury College, Middlebury, VT, an MS in Physiology and MD degrees at the University of Hawaii, Honolulu, HI where he grew up. He trained at Mayo Clinic Rochester and is Board Certified in Internal Medicine, Subspecialty Pulmonary Disease, Critical Care Medicine, and Sleep Medicine. He has been at Mayo in his current position for 36 years now. He has been dedicated to regulatory advocacy efforts, research and clinical care in support of patients with various disorders leading to chronic hypercapnic respiratory failure.
William Noah, MD, is the Medical Director of Sleep Centers of Middle Tennessee, which has multiple clinic locations, including Murfreesboro, Franklin/Nashville, and Clarksville. He also founded OSAinHome, a comprehensive solution for sleep apnea testing, and is a founding member of the Middle Tennessee State University Sleep Research Consortium.